Pandemic focus shows way for pharmacy
In Running Your Business
Follow this topic
Bookmark
Record learning outcomes
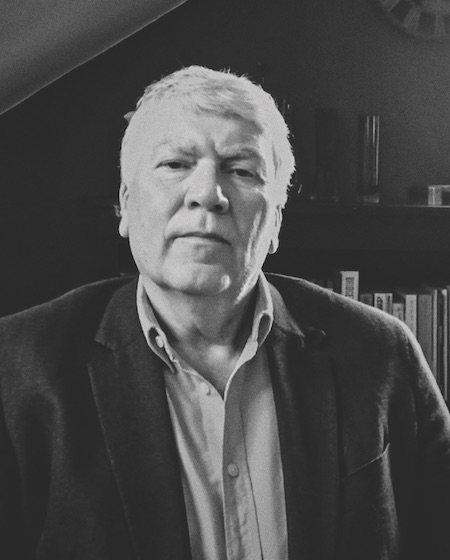

Cegedim’s strategic business development director Gian Celino (right) says he has been spending more time since the pandemic was declared engaging with the national bodies that look after primary care and general practice. “Covid has brought about a focus: ‘do this one thing, and do it well’,” he says. “Keeping that orientation towards action and results would be brilliant; we are getting things done in no time at all that previously would have taken months to agree, and possibly years to deliver.”
That “one thing” has been creating capacity in the NHS, he says. Decisions taken to “protect the NHS and save lives” prioritised capacity building in intensive care. Everything else was pushed back down the system. GPs were focused on ensuring infected patients got into hospital when they needed to. Regular GP work was triaged to remote consultations and non-urgent conditions were excluded from general practice altogether. Many of those people ended up in pharmacy.
“We’ve made bricks and mortar unimportant, and at the same time we’ve made it very important,” Mr Celino says. “Having a physical encounter is important, depending on your problem or concern, but if you don’t need a physical encounter, there are lots of different ways you can engage with the NHS, with general practice, with pharmacy.
“That’s a great opportunity, but it has exposed considerable weaknesses, given where pharmacy finds itself. New models, like doctors working remotely, are emerging, but we are all tolerating a certain clunkiness because it’s urgent. That clunkiness is not sustainable in the long term. Technology has a tremendous amount to do to make this far slicker, for patients, clinicians and the health system as a whole. That’s where a lot of our [Cegedim’s] attention is at the moment.”
Return to normal, or transform?
Gian Celino started his career in community pharmacy. He says the experience of the past three months has created a great and immediate opportunity to change things for the better in the sector. He asks: “Do we return to what is familiar, or use this opportunity to transform to become properly part of the health care ecosystem?”
Group managing director Steve Bradley (left) says Cegedim takes a systems view. “We think less in terms of community pharmacy systems and GP systems, and more in terms of healthcare systems that have different capabilities depending on what you want them to do.”
He says it also helps to consider things from the patient perspective. “The whole media focus has been on the NHS doing a fantastic job, but patients have had to navigate a disjointed system. They are told to see their pharmacy. The pharmacist says ‘this is more appropriate for your GP’. When we get to any sort of normality, patients are going to expect a much smoother process. Digital solutions can help with a lot of that.”
“We know from working with general practice that you get nowhere without a capacity and demand model,” Gian Celino says. “We want general practice to be able to do more for patients to take demand off secondary care. In turn, general practice needs pharmacy to do more to take demand off them. There are lots of barriers to that, but one of the most fundamental is the ability of general practice to refer a patient to a pharmacy and vice versa – and not just into a black hole. It’s booking an appointment, knowing who they will see, when and where, and finding out what happened. It’s got to feel like sending them to the nurse or pharmacist in the practice. It’s security of the continuum of care.
“GPs will need that to be completely satisfied, as they’re the nexus for the patient’s care,” he explains. “If someone else is providing care to their patient, they don’t need to be in control of it, but they do need to be assured of it. We don’t have a practical model for that yet in pharmacy, but there are technological models all over the place. It’s the bread and butter of doctors and consultants exchanging information.”
Mr Bradley says that Cegedim has had an idea on the drawing board for over a year. “A piece of technology that allows seamless two-way referral and dialogue to take place between pharmacy and general practice. We’d love to build something like that, as we have done already for optometrists, but we struggle at the moment to identify who really wants it, and the funding side is a challenge too.
We can blame the politics, the direction of travel, but you only have to look across the border in Scotland to see how things can be different
“You’re not talking millions, but it will cost many thousands. It depends how complex you want the solution to be. A pharmacy might see a patient who’s been referred by their GP, but what’s the next point the pharmacist refers on to? The more endpoints, the more complicated the project becomes.”
Gian Celino says he doesn’t see any evidence of a wholesale understanding of this demand management conundrum across the national pharmacy organisations, at least not in England. “We say the funding model is wrong, that supply is still the tail that wags the dog, that the technology isn’t there. But we say that the biggest waste of resources is to build a technology for a problem nobody wants to solve,” he says. “The problem and solution have to be hand in hand. We can blame the politics, the direction of travel, but you only have to look across the border in Scotland to see how things can be different.
He says everybody needs to play a part in bringing together a set of ideas with a will to do something. “Policymakers, us technology people, the community pharmacy workforce, pharmacy owners need to say ‘let’s do this’. That ‘call to action’ happened with Covid. In general practice, in community pharmacy, people have just got on with it, and done it because it’s been the most important problem they’ve had to solve. We need to make changing what we do in community pharmacy the most important problem we have to solve.”
A lack of joined-up thinking
Steve Bradley says the way other organisations are set up doesn’t help either. “Take NHS Digital,” he says. “We deal with a completely different team in the pharmacy space to the GP space. There does not seem to be any joined-up thinking at that level, or above that level.
“The primary care team in NHSE will say ‘that’s interesting, go and talk to the pharmacy team’, who will say ‘that’s very interesting’. But nobody seems to want to get behind anything. The challenge is that if we build something, a national body could turn round in six months’ time and say ‘that’s very good, but that’s not what we want’.
“There are some good examples in Scotland where community pharmacy and general practice have worked together. It’s partly driven by geography, but also by innovative pharmacists trying to break the mould, providing an increasing range of services to patients, who work hard at demonstrating their capabilities to get GPs on board.
“If you tried to replicate that across the UK, it would take years to get to the point it was working. It needs some centralised steering group to take four or five examples and say ‘let’s see how we could roll this out into the wider community’. Cultural change and patient education done at a local level will be very costly and time-consuming, but initiatives run from the centre can point things in the right direction. We don’t necessarily need one size fits all, maybe its four sizes for the different UK markets, but we don’t want hundreds of ways of doing things.”
“We are fortunate to have lived through Covid, for all its drawbacks,” says Gian Celino. “It’s exactly the sort of shock that leads to something good, but equally, it’s like betting black or red at the roulette table. We could just go back to what we were doing before, and live to regret it.”
