Plugging the gap: How Pharmacy First contributes to primary care
In Views
Follow this topic
Bookmark
Record learning outcomes
Leela Barham looks at workforce modelling for primary care in England and highlights pro bono work from consultancy Frontier Economics that has explored the potential contribution of Pharmacy First in meeting demand
It’s no surprise to hear that workforce modelling suggests demand for primary care in England is going to outstrip supply in the future. But in a change to previous workforce modelling efforts, Frontier Economics has explicitly modelled the difference that Pharmacy First could play in plugging the gap. And they even did the work for no charge.
The National Audit Office said in its independent assessment of NHS England’s (NHSE) modelling that underpinned the Long Term Workforce Plan (LTWP) that workforce modelling is an “evidence-based and transparent tool for beginning a conversation, including with different stakeholders, about the desirability and feasibility of different approaches and policies.” Better to be forewarned...
Rising demand
Shortfall in GPs
As part of its modelling efforts, NHSE looked specifically at the GP workforce. It concluded that without change, there would be a shortfall of GPs in the future. That’s the conclusion that consulting firm Edge Health also came to and Frontier Economics’ modelling comes to the same conclusion.
Pharmacy First could help
There’s a lot that could help to fill the gap between the demand for primary care and the supply from GPs. NHSE has already committed to increasing GP speciality training places, for example. Edge Health suggested this alongside efforts to retain GPs, increase other staff in primary care, cut demand in the first place by targeting the prevalence of obesity and diabetes and use innovation. All good stuff. No mention of community pharmacy though in helping to manage the challenge.
It’s not that NHSE hasn’t considered the community pharmacy workforce. It’s just that this is done separately.
Edge Health did its work in 2022, so that was before Pharmacy First was in place. Again, this was undertaken on a pro bono basis – so in the interests of pragmatism it was focused on GP data as the key data source. The work was done to “showcase how workforce modelling can help inform decision-making,” according to Lucia De Santis, senior analyst at Edge Health.
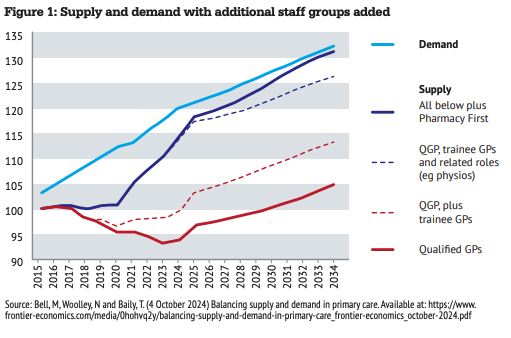
Frontier Economics’ workforce modelling not only looks at using other staff in primary care as well as direct patient care roles through the Additional Roles Reimbursement Scheme, but also at Pharmacy First. That could get supply much closer to demand by 2034 (see Figure 1).
Frontier Economics assumes that Pharmacy First could have the effect of adding one million consultations per year before it reaches 10 million a year in 2034. That’s equivalent to 1,631 full-time equivalent qualified GPs. Pharmacy First has not been without problems, and Community Pharmacy England has taken aim at policies that it says are based on abstract modelling without considering what is achievable in the context of a struggling pharmacy sector. Whether the service could really deliver that much activity is not a given.
Quantified value
It’s not news that community pharmacies could play a role in helping the under-pressure primary care sector in England. But it is useful to have workforce modelling that sets out just what a difference the sector could make through Pharmacy First; it’s not just warm words, it’s quantified, even if uncertain. It’s another way to show the real value of community pharmacy.

