Screen test: BP gets fit for pharmacy
In Pharmacy In Practice
Follow this topic
Bookmark
Record learning outcomes
Norman de Villiers is on a mission. The South African pharmacist’s Medi-Stats BP+ programme, which is being introduced via pharmacy ahead of other locations, “allows AF to be detected, hypertension to be understood, patients to be engaged and treatment to be approached in a preventative manner”.
The Medi-Stats BP+ in many respects resembles a normal blood pressure device, but it captures brachial blood pressure plus a range of additional information to assist interpretation of cardiovascular health. The Medi-stats portal, developed by Norman and his team, provides the kind of output that anyone who had a £1,000 medical 10 years ago might recognise, but whose neat lines and colour coded graphs and charts are not normally found in community pharmacy consultation rooms. The package is designed to make an impact in a number of ways.
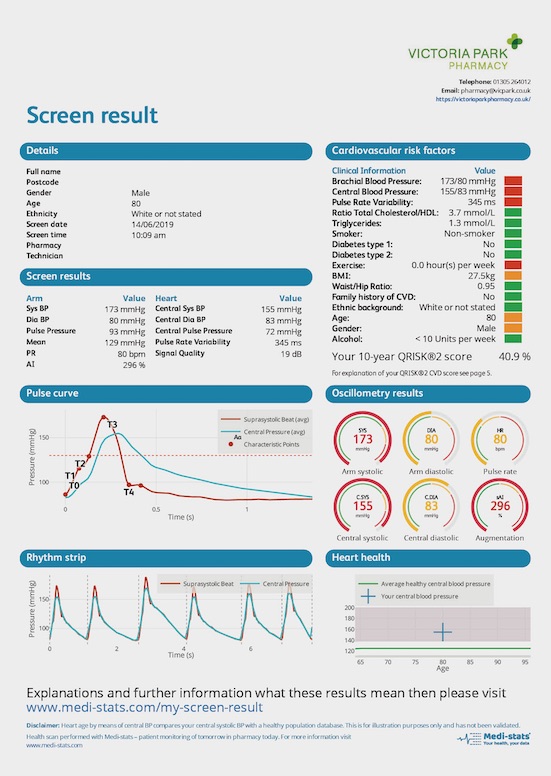
“You normally only see the heart rate, systolic and diastolic pressure for your arm,” Mr de Villiers says. “Our machine gives you a central aortic blood pressure too, pulse rate variability, which picks up any rhythm disturbances – if this is above 100 we will refer you for an atrial fibrillation check – the augmentation index (AI), which reflects how stiff the arteries are, and we look at pulse pressures, which is one of the new cardiovascular risk factors. We follow NICE guidelines, but we have additional bits that we follow too.
“Quite a few people are moving to use central blood pressure,” he says, “which is the pressure that affects your internal organs. Because that is affected differently by medication, what we are finding with our cohort studies is that you miss people if you are only looking at arm pressure. Too high blood pressure centrally can kill you. I’m working with UCL so we can build a database to see if we can persuade NICE to include this down the line. It’s the way to go.”
We like to get the patient involved. They can change and adapt data and see their progress
Patients complete an online health history at home to save pharmacy time, leaving the pharmacy team to manage the results and cardiovascular health at the time of the appointment. The results of the BP checks are available in 60 seconds, allowing rapid retest. “I normally find after the second one, as people start to get used to the feeling, it’s already improved, and with the third one people are where they should be,” Mr de Villiers says. The test results are then combined with factors from the questionnaire on a series of screens, colour coded to aid understanding.
This includes:
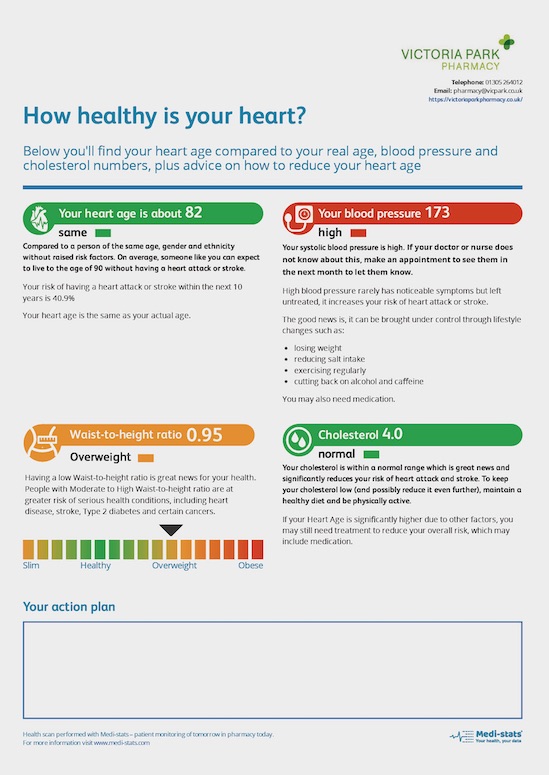
- A heart age and blood pressure summary, with health advice if needed, along with a waist to height ratio with health scale and a cholesterol value if available, as well as a record of any action plan agreed
- The screen result, showing colour coded cardiovascular risk factors, a visual pulse curve and rhythm strip (a 10 second snapshot of how the heart is pumping), and a heart health graph based on the central BP reading (validated, but not yet included in NICE guidelines)
- A record of the medical questionnaire, which incorporates GAD 7 (the Generalised Anxiety Disorder) score and the PHQ 9 (Patient Health Questionnaire depression test score) and a validated QRisk®2 result.
The results can be emailed to a cardiologist, to the patient, or a GP as well as used in the consulting room during the screen process. Data can be transferred directly to PharmOutcomes during health checks. Patients have access to their own data on a smartphone, empowering them to manage their own health. “Every time a patient visits, the data is locked into the system. We like to get the patient involved. They can change and adapt data and see their progress.”
Mr de Villiers says patients with adverse findings can see results quickly, with the added benefit of watching their own metrics change, almost in real time. He provides an example related to an adverse finding in the pulse curve, showing a lag in the central pressure return after a beat, indicating a degree of arterial stiffness. “You can send people away with advice to walk with variable pace to get the heart rate up for 20 minutes a day, you get nitric oxide formation in the endothelium of the artery and it makes it relax. That makes the whole heart calm down. Do that over a period – when you are older it can take three months – but I’ve found with a lot of guys even after two weeks, they can see how the pulse curve changes. When people don’t believe me, I say walk around the block and come back and see me and I will show you.
“We need to get the arteries to relax, and this is what blood pressure medicines like ramipril, calcium channel blockers and ARBs do; they vasodilate. This is why applying this as part of the New Medicine Service works so well. This is you today; you’ve been prescribed your medicine. The GP says your blood pressure is high. Take it, come back in a week and then again in two weeks’ time – footfall back into pharmacy – and the patient can see what the medicine is doing. This is where I see the adherence increase, because now it makes sense to the patient.
Examples of patients referred
 • A 74-year-old female with high CV risk, undiagnosed hypertensive. The patient did not take the traditional BP check seriously and only agreed to the referral after the in-depth knowledge exposed her CV health and she could see the additional load on her heart function.
• A 74-year-old female with high CV risk, undiagnosed hypertensive. The patient did not take the traditional BP check seriously and only agreed to the referral after the in-depth knowledge exposed her CV health and she could see the additional load on her heart function.
• An 82-year-old male whose blood pressure was managed after instigated 15-minute variable pace walking advised during a New Medicines Service – brachial systolic pressure reduced from 132 to 119mmHg. He now regularly cycles and goes for walks.
• A 53-year-old male hypertensive male prescribed amlodipine and ramipril. Two days prior to the screen he had stopped his amlodipine due to swollen feet and ankles. After daily screens to monitor BP and illustrate the effects of non-adherence, the patient resumed amlodipine on day six, became more engaged and now endeavours to exercise more regularly.
“This provides a lot more understanding of what a medicine is doing, and that is what I saw the first time and I thought ‘if we can capture this for pharmacy, we give pharmacy that position in the referral pathway where we can provide a service in passing information onto the GP (and the patient): this is what you are achieving,’ hopefully we can win like that.”
He says it is important we have a greater understanding of the differences between brachial and central blood pressure. It could explain some of the side effects, such as swollen ankles with amlodipine we encounter.
Mr de Villiers has been trialling the service for one or two days a week in Victoria Park Pharmacy in Dorchester for months – the version one pilot was in 2015/16 – with the device used to support NMS and MURs as often as possible on those days. News of the service has spread, and patients are now being charged for the service, at £30 for a 30 minute full check, and £10 for a recheck (10-15 minutes) “There was a stage during the research where we didn’t charge them, if it’s a New Medicine Service or MUR once a year I can do this for you and the NHS pays, but if I do a recheck for you, then that will cost you £10.”
Functionality continues to develop
Victoria Park owner Robin Mitchell says: “We’ve been a bit of a guinea pig for Norman. The equipment functionality has been there from the start, the AF detection and pulse curve have come along since. I don’t consider myself an expert; I tend to look at it as a blunt instrument that gives some real added value.
“From the pilot studies we got a sense of what was different. It’s a blood pressure monitor, but it does some additional things. We’ve rolled along using it in different ways. As a pharmacist in a community pharmacy, what I am interested in is how a technology like this can be used efficiently, including how data is gathered.
“I buy into the value of it in a number of ways. It’s a clever piece of kit that tells you things that other bits of kit can’t tell you easily in a pharmacy environment, combined with an interface which produces elegant analysis of the cause. Patient response in my experience is very good – the reporting can be a bit more complicated than some patients want; others have a level of understanding that they want to get into the subtleties. In general, the ability to dig in a bit further, looking at your central pressure, arterial stiffness and pulse rate variability, we can paint a much more nuanced picture and that’s what I like about it.
It’s a clever piece of kit that tells you things that other bits of kit can’t tell you easily in a pharmacy environment
“In an ideal world, I’d be using this as part of a locally commissioned service, so that when patients are newly diagnosed with a cardiovascular issue, and you put them on new medicines, we monitor patients for a period of time and see how the medicines are behaving. We’ve seen our share where the blood pressure goes down, but the central BP comes down too much and people are reporting dizziness or wobbliness etc. We’ve got as far as contacting the Clinical Commissioning Group and the progressive consultant cardiologist up the road is keen on interfaces between primary and secondary care, so we have a local committee open to the idea of looking at the technology with a view to scoping a service and running a pilot.”
If so, how does it relate to the priorities in Dorset?
“AF seems to get a lot of traction, and we’ve picked up several cases of that, but in my mind that’s not the sweet spot for this product. The good news is that with the new contract and GP directed enhanced services, there should be more opportunity to look at this and pull it through and engage with GP pharmacists who might appreciate this better and work through it. If it hits somewhere, I think it won’t be too long before people want to take another look.
“There are two buckets for this. One as an integrated part of care pathways, the other is the health check, helping people understand their health and own it more, and the visual detail that comes out of this is generally very helpful and well received.”
