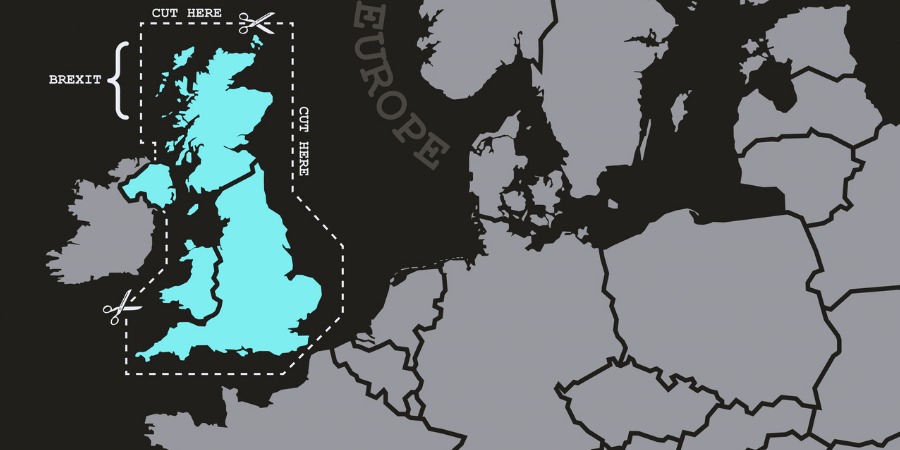
Brexit, Brexit and community pharmacy's future
In News
Follow this topic
Bookmark
Record learning outcomes
Minister ‘confident’ in Brexit contingency planning
Health Minister Stephen Hammond says that even if the UK leaves the EU without a deal, he is confident the work done across the supply chain will guarantee continuity of medicines supply.
Speaking at the Health Distribution Association Conference last week, Mr Hammond thanked the Association’s members for their “constructive” support over recent months, which he said had been some of the most challenging in peacetime history. "I am sure we have taken the necessary steps to ensure patients will have access to the medicines they need", he said, adding that he recognised that shortages are not all due to Brexit.
The Minister added that he understood the challenges and frustrations related to FMD, and he acknowledged the work HDA members had done to provide data in respect of the new legal obligations related to medicines pricing. He said: “The NHS Long Term Plan sets out a funding increase for the NHS, a new service model, priorities for outcomes, and provides a strategy for how technology can improve care and safety." But he also recognised that the NHS will be tested in future as never before.
The work on Brexit planning was acknowledged by HDA chief executive Martin Sawer, who said the association had been working for other stakeholders for many months on contingency planning, including in the event of ‘no deal’. But he had a warning to the Government related to the ongoing situation. "The uncertainty associated with Brexit is not scaremongering. Our members need to invest in new generation technology; this holding pattern can only go on so long,” he said.
That view was echoed by ABPI chief executive Mike Thompson. Noting that 45 million packs of medicines are exported to the EU each month, with 37 million packs coming in the opposite direction, Mr Thompson said: “No deal was pretty close in March or April, so the delay has been welcome. But it takes time to reorganise supply chains; a solution which is 80 per cent OK may be fine for some sectors, but is not fine for us. We need 100 per cent of patients to get the medicines they need.
“We are the best prepared sector, and we intend to stay the best prepared sector,” he continued. “If ‘no deal’ remains a scenario, then we believe additional ferry capacity will be required. The best way to avoid the disruption to medicines supply, is to leave with a deal in place.”
Community pharmacy ‘on its knees’
“There is no more money to be squeezed out of community pharmacies,” Pharmaceutical Services Negotiating Committee chief executive Simon Dukes told the Conference. "Many community pharmacies are now using reserves they will need in the future for investment to deliver those services in the NHS Long Term Plan they want and patients need."
He said there is an appetite across the country for change. “The Government wants value for money, medicines safety, and an increase in urgent care and minor conditions, and prevention in an integrated way with primary care networks. There’s a lot to fit in, but fair remuneration for services is essential."
Stressing the need for collaboration within the sector, Mr Dukes said that this would mean exploring new business models, including those that had been problematic in the past, such as hub and spoke, and consolidation of pharmacies. “All will have implications for distributors,” he said.
Confirming PSNC was seeking a multi-year deal, Mr Dukes said: "We have an ambitious Long Term Plan - 10 years - and ambitious change with the GP contract. There are some real challenges in upskilling, investment and a change programme to deliver. That’s not something you can do in one, two or three years."
He also signalled a more inclusive approach as talks progress. “There is a need to bring the National Pharmacy Association, the Company Chemists’ Association and the Association of Independent Multiples into talks as negotiations progress. Ultimately their members have to deliver whatever we have as a settlement. The contract needs to be one they all feel they can deliver on."
Mr Dukes said community pharmacies need to think about primary care networks. “On average they [PCNs] will have 10 -15 community pharmacies. That, to me, seems like an opportunity. They need to talk to each other about what their offer might be. LPCs can start talking to LMCs about how they work together, to resolve disputes on the ground. It’s time to set out what we can deliver.”
Early indications good for DMIRS and NUMSAS
Pharmacy has opportunities in a number of areas, including new service models, local commissioning and co-operation to plan population health around whole patient pathways, says deputy chief pharmaceutical officer Bruce Warner.
He said early evaluations of the Digital Minor Illness Referral Service (DMIRS) and the NHS Urgent Medicines Supply Advanced Service (NUMSAS) were “very promising”, Dr Warner said community pharmacy has the capacity to deliver more clinically focused care and that Primary Care Networks (PCNs) are “a real opportunity to make a massive difference.”
The timetable is rapid. PCNs by July, the second national plan for antimicrobial resilience by the end of 2019/20, 20,000 extra staff including pharmacists, in PCN-based multiprofessional teams, and the new GP contract including a quality improvement module on prescribing safety. “We don’t have money to waste,” Dr Warner said. “We still have up to 8 per cent of patients in hospital because of medicines issues. We need to make sure that patients are only taking medicines that are actually doing them some good.”
He added: “Pharmacy and pharmacy staff being asked to do what GPs might have done in the past is a good thing, but all team members will need to operate towards ‘the top of their licence’.”
Chair unveils plan for new five year strategy
 The HDA is developing a new five year strategy, designed to remedy concerns that the role distributors play is still not fully understood. “This means massive gains in productivity are not recognised, neither are costs, in regulation or investment,” chair Jeremy Main told the conference. The strategy, which will build on the outputs from recent stakeholder research conducted by the association among manufacturers, pharmacists and regulators/payors, will be unveiled later this year. Its key themes are likely to include deeper engagement with stakeholders, broadening communication about the role and value of the distribution sector, and thought leadership as the sector changes and evolves, including acting as a convenor of cross sector discussions of issues of mutual interest.
The HDA is developing a new five year strategy, designed to remedy concerns that the role distributors play is still not fully understood. “This means massive gains in productivity are not recognised, neither are costs, in regulation or investment,” chair Jeremy Main told the conference. The strategy, which will build on the outputs from recent stakeholder research conducted by the association among manufacturers, pharmacists and regulators/payors, will be unveiled later this year. Its key themes are likely to include deeper engagement with stakeholders, broadening communication about the role and value of the distribution sector, and thought leadership as the sector changes and evolves, including acting as a convenor of cross sector discussions of issues of mutual interest.
Mr Main is the first fully indepedent chair in the HDA's 152 year history. He held the role twice before as a member representative, during his time at Alliance Healthcare.
In brief
 The implementation of the new security features in the Falsified Medicines Directive has already uncovered counterfeits circulating in Holland. “We need to be vigilant”, says HDA chief executive Martin Sawer. He said all Wholesale Dealer Authority licence holders should be held accountable to the same standards. The HDA estimates that more than two thousand premises are not yet registered with the authorities. He said the same applied to new technologies that might open up efficiencies, such as hub and spoke and central dispensing operations. "Online pharmacy should be subject to the same standards as HDA members are now,” he added.
The implementation of the new security features in the Falsified Medicines Directive has already uncovered counterfeits circulating in Holland. “We need to be vigilant”, says HDA chief executive Martin Sawer. He said all Wholesale Dealer Authority licence holders should be held accountable to the same standards. The HDA estimates that more than two thousand premises are not yet registered with the authorities. He said the same applied to new technologies that might open up efficiencies, such as hub and spoke and central dispensing operations. "Online pharmacy should be subject to the same standards as HDA members are now,” he added.
Support for PSNC’s determination to secure a multi-year deal in the contract negotiations were are now underway came from the ABPI’s Mike Thompson. “I’m surprised that pharmacy negotiates every year. Some certainty over a period of time would seem sensible to us,” he said, noting that the pharmaceutical industry had recently signed up to the new Voluntary Pricing and Access Scheme (VPASS), which will cap sales growth to the NHS to 2 per cent per year for each of the next five years.
Medicines shortages peaked at 313 issues in January 2019. An internal government Medicines Shortage Response Group is now providing oversight, particularly of management plans designed to deal with
Award for the best line of the day went to ABPI chief executive Mike Thompson. “Brexit feels like a period of history, than any particular outcome. A time with a plot line more complicated than Game of Thrones, and a Parliament with a cast of characters destined to be known as the Brexit generation.”
The UK has done better than many other European countries in getting FMD off the ground on time, according to Mr Thompson. And he had a warning for those who might assume the end of FMD after the UK leaves the EU. “Counterfeiters are getting increasingly sophisticated in their approach to the market. It would be unacceptable for the UK to be the only country in the region without this system".
Blunt assessment from North East London Local Pharmaceutical Committee chief officer Hemant Patel: “The community pharmacy model, with 95 per cent of income from dispensing, is dead,” he told the conference, before suggesting local provider models and a range of local contracts for different integrated, immediate care and prevention services were the future.
