In Running Your Business
Follow this topic
Bookmark
Record learning outcomes
In what’s been described as the biggest shake up in the NHS in more than a decade, the Health and Care Act 2022 aims to improve health outcomes by joining up NHS, social care and public health services at a local level and tackling growing health inequalities.
Formally merging NHS England and NHS Improvement, and giving the secretary of state for health and care powers of direction over national NHS bodies and local systems and trusts, the majority of the Act centres around developing system working by putting integrated care systems (ICSs) on a statutory footing through the creation of integrated care boards.
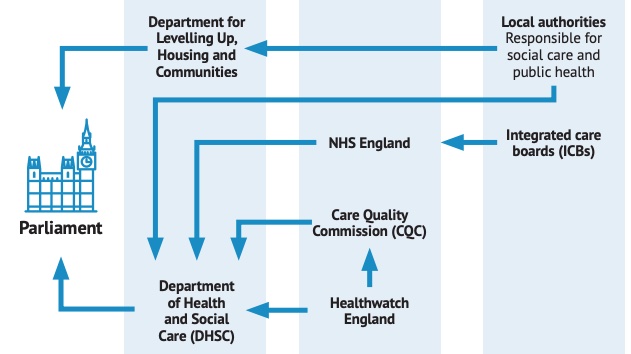
But with a range of national bodies now involved in shaping and operating England’s health and care system, just how do their core responsibilities and accountabilities fit together?
Central government departments
The Department of Health and Social Care (DHSC) and the Department for Levelling Up, Housing and Communities (DLUHC) lead the oversight of and hold accountability for health and social care.
With responsibility for policy, legislation, funding and delivery of health and care in England, DHSC’s main objective is to “lead the nation’s health and social care to help people live more independent, healthier lives for longer”.
When Public Health England was disbanded in 2021, DHSC took on its health improvement function; its health protection functions moved to the United Kingdom Health Security Agency (UKHSA), and responsibility for health promotion, health improvement and addressing health inequalities fell to a new directorate within DHSC called the Office for Health Improvement and Disparities (OHID).
DHSC has oversight of a range of executive agencies and non-departmental public bodies, collectively known as arm’s-length bodies (ALBs), such as the Medicines and Healthcare products Regulatory Agency (MHRA). Framework agreements set out how they work together and how ALBs will be held to account.
DHSC also has responsibility for the delivery of local government’s public health and adult social care functions, although not the related spending or auditing. Responsibility for these falls to another central government department, the Department for Levelling Up, Housing and Communities (DLUHC – formerly the Ministry for Housing, Communities and Local Government).
DLUHC also allocates resources and audits spending on the other services delivered by local authorities. If a local authority is failing to deliver services or use public money correctly, the secretary of state for DLUHC can take over.
NHS England
As well as introducing significant change at system level, the 2022 Act also realigned national accountabilities, incorporating NHS Digital, NHSX, Health Education England and NHS Improvement into NHS England, which is now responsible for providing national leadership and direction for NHS organisations in England.
As the largest of DHSC’s arm’s-length bodies, NHS England has a budget of £147.8 billion for 2022/23. Accountable to Parliament, it is led by a board, with annual objectives set by the secretary of state for health and social care via the NHS Mandate.
NHS England’s overarching role is to support England’s health service by funding integrated care boards (ICBs) to arrange and commission services for their local populations, as well as commissioning some specialist services itself. In consultation with the Government, NHS England also produces annual operational planning guidance for ICBs, with operational and financial performance monitored by NHS England’s regional performance managers to ensure delivery.
Other arm’s-length bodies
Additional ALBs responsible for quality, safety, standard setting and public involvement include:
• The Care Quality Commission (CQC) – the independent quality regulator for health and adult social care in England. Led by a Board, the CQC’s regulatory functions are funded by DHSC and by registration fees paid by all regulated health and social care services providers. The CQC is accountable to Parliament and to DHSC, and has oversight of Healthwatch England
• Healthwatch England’s core function is to provide leadership, advice and guidance to local Healthwatch organisations, who gather public views and insights about health and care services. The local bodies are funded by and accountable to local authorities. The chair of Healthwatch England is appointed by the secretary of state and sits on the CQC board, although Healthwatch England has budgetary and operational independence
• The Healthcare Services Safety Investigation Branch (HSSIB) will become operational in April 2023 as a division of NHS England. Accountable to DHSC, it replaces the Healthcare Safety Investigation Branch (HSIB) in investigating incidents of poor care that have an impact on patient safety
• The National Institute for Health and Care Excellence (NICE) is funded by DHSC and is accountable to Parliament. Its responsibility is to set standards for health and social care practitioners, commissioners and managers, covering the clinical and cost effectiveness of medicines, medical devices and medical procedures.
Integrated care
Integrated care systems (ICSs) bring together NHS organisations, local authorities and other service providers to work collaboratively to improve population health, reduce inequalities, enhance productivity and value for money, and help the NHS to support broader social and economic development.
ICSs evolved from sustainability and transformation plans/partnerships (STPs) formed in 2016 to develop ‘place-based plans’ for health and care services in their areas. Subsequently formalised as legal entities with statutory powers and responsibilities in the 2022 Act, there are currently 42 ICSs across England, serving geographical populations of between 500,000 and three million people.
ICSs have two key elements:
- Integrated care boards (ICBs) are responsible for allocating the NHS budget and commissioning services. Directly accountable to NHS England, they cover the functions previously held by clinical commissioning groups (CCGs) and some of the direct commissioning of NHS England. ICBs operate as unitary boards, with membership including (as a minimum) a chair, a chief executive officer and at least three others drawn from NHS trusts and foundation trusts, general practices and local authorities in the area. Each ICB must prepare a five-year system plan setting out how it will meet the health needs of its population, giving regard to partner ICP’s integrated care strategy and informed by the joint health and wellbeing strategies published by the health and wellbeing boards (HWBs) in its area. The ICB and its partner NHS trusts must develop a joint plan for capital spending on buildings, infrastructure and equipment within the geography
- Integrated care partnerships (ICPs) are statutory joint committees of the ICB and local authorities in the area. ICPs bring together system partners to develop an ‘integrated care strategy’ to address the wider health care, public health and social care needs of the population. This strategy must build on local joint strategic needs assessments (JSNAs) and health and wellbeing strategies, developed alongside local communities and Healthwatch.
ICSs are expected to achieve financial balance and meet national requirements and performance targets, and are accountable to NHS England via their ICB.
Primary care
Primary care networks (PCNs) are groups of GP practices which, since April 2019, have come together with other healthcare staff and organisations to provide integrated services locally, covering populations of 30,000 to 50,000.
From April 2020, the Network Contract Directed Enhanced Service (which sets out core requirements and entitlements) has required general practices, as part of their PCN, to collaborate with non-GP providers, such as community pharmacies. Every ICS has a critical role in ensuring that PCNs work with other community staff and use multi-disciplinary teams across primary and community care.
Local pharmacy structures
Local pharmaceutical committees (LPCs) work locally with NHS England area teams, PCNs, local authorities and other health professionals to help plan healthcare services. The LPC discusses and negotiates pharmacy services with commissioners and liaises closely with its medical, dental and optical equivalents.
There are around 70 LPCs, although this is set to change following the Wright Review into pharmacy representation which proposed increasing efficiencies by – amongst other measures – reducing the number of LPCs, a proposal supported by a subsequent contractor vote, but which has not yet been put into practice.Health and wellbeing boards
Established in 2013, health and wellbeing boards (HWBs) continue to play a key role in driving joined up working at a local level and setting the strategic direction to improve the health and wellbeing of people locally, alongside ICBs and ICPs.
Each local authority (including London boroughs) is required to have an HWB, which must include a representative from each relevant ICB. HWBs may choose to invite other organisations from the voluntary, community and social enterprise (VCSE) sector, children’s and adult social care, and other healthcare providers to join them.
As a forum for discussions about strategic and operational co-ordination in the delivery of services, HWBs are responsible for assessing the health and wellbeing needs of an area and publishing a joint strategic needs assessment (JSNA) and a joint local health and wellbeing strategy (JLHWS) that sets out the priorities for improving the health and wellbeing of the local population, and how the assessed needs will be addressed, reflecting the JSNA evidence.
JSNAs and JLHWSs are not an end in themselves, but a regular process of strategic assessment and planning. NHS England, local authorities and ICBs are required to have regard to the relevant JSNAs and JLHWSs when exercising their functions. Each HWB also has a separate statutory duty to develop a Pharmaceutical Needs Assessment (PNA) for their area.
A PNA is a statement of the need for pharmaceutical services, including those provided by dispensing appliance contractors and dispensing doctors, and is used by NHS England to determine whether to approve the opening of new NHS pharmacies in an area. The PNA analyses the population’s health needs, identifies any gaps in service provision and provides intelligence to create, improve or provide better access.
The PNA is part of the overall planning for health and social care in the health and wellbeing board area, should be integrated with the JSNA and includes risks to health and wellbeing. A PNA cannot be subsumed into a JSNA or JLHWS, but can be annexed to them.
Simply complex
If it seems as if all these departments and bodies are mechanisms to spread decision-making and accountability wider, it’s worth considering the times we are living in. Since the NHS was set up in 1948, its focus pivoted from treating single conditions to meeting the complex health and care needs of a population that is living longer, yet not healthier lives.
“As a consequence,” says The King’s Fund, “people too often receive fragmented care from services that are not effectively co-ordinated around their needs [which] can negatively impact their experiences, lead to poorer outcomes and create duplication and inefficiency”.
The solution to better care that meets people’s long-term health needs, comes from a joined-up approach that unites primary and community health and social care in collaborative working to address growing health inequalities.
“Health inequalities are wide and growing”, continues the Fund, “but they are not inevitable, as evidence shows that a concerted approach, combining the NHS and wider policies to address the social and economic causes of poor health, can make a difference.”
One, two, three
ICSs are expected to work through smaller geographies known as 'neighbourhoods', 'places' and 'systems':
Neighbourhoods are groups of GP practices working with NHS community services, social care and others to deliver co-ordinated and proactive care, including through PCNs and multi-agency neighbourhood teams.
Places are partnerships of health and care oganisations in a town or a district to join up the planning and delivery of services and redesign care pathways, engage with local communities and address health inequalities.
Systems comprise health and care partners working at scale to set overall system strategy, manage resources and performance, plan specialist services, and drive strategic improvements on workforce planning, digital infrastructure and estates.